Digital Health, the new global paradigm for the transformation of the health systems
Digital Health is the new global paradigm for providing effective, equitable, high quality health services with great human sensitivity that allows for connecting people and their family with health units and their community.
Progressively it will be consolidated in the different spheres of health in Latin America and the Caribbean, privileging proactive prevention and the timely detection of risk factors to thereby favor a timely diagnosis that, supported by the use of the digital platforms, permits precise and high quality treatment to help more people live longer and better.
With this vision in mind, the Carlos Slim Foundation has created the Portal de Salud Digital, where we join forces so that the different health professionals that participate in the generation, development, implementation, evaluation and scaling of the Digital Health solutions as public policies have a universe of knowledge within their reach, whether through their computer, their cell phone or their tablet.
The value of Digital Health
Digital Health is the new global paradigm in health that has been adopted by the World Health Organization,1 the Pan-American Health Organization,2 the Broadband Commission for Sustainable Development3 and the Inter-American Development Bank,4 among others. Digital Health is the catalyst for the transformation of health systems and makes it possible to provide innovative, effective, equitable and high quality services and interventions. Digital Health also connects patients, their family and their community in prevention, timely detection, precise diagnosis and continuous care. Finally, Digital Health enables the follow up and monitoring of the health services provided, promoting transparency and accountability, and laying the foundations for the formation of a verifiable health system.
What is Digital Health?
Digital Health is defined as the convergence of four disruptive trends, powered by Artificial Intelligence:5
⦁ The use of digital platforms, with integrated expert systems that support decision making based on evidence.
⦁ Cloud-based services, with robust infrastructure the enables the transactionality of large volumes of information or big data.
⦁ Mobile Apps and the Internet of Things, which permit self-monitoring, remote monitoring and adherence to a healthy lifestyle.
⦁ Social networks and connected communities, to facilitate the connection with patients, their family and their community.
Change of paradigm: personalized public health
Digital Health catalyzes personalized public health6 and is expressed through the “wheel of health” characterized by 6Ps:
⦁ Proactive, with strategies accessible to the person in the community and at home for the evaluation of risks.
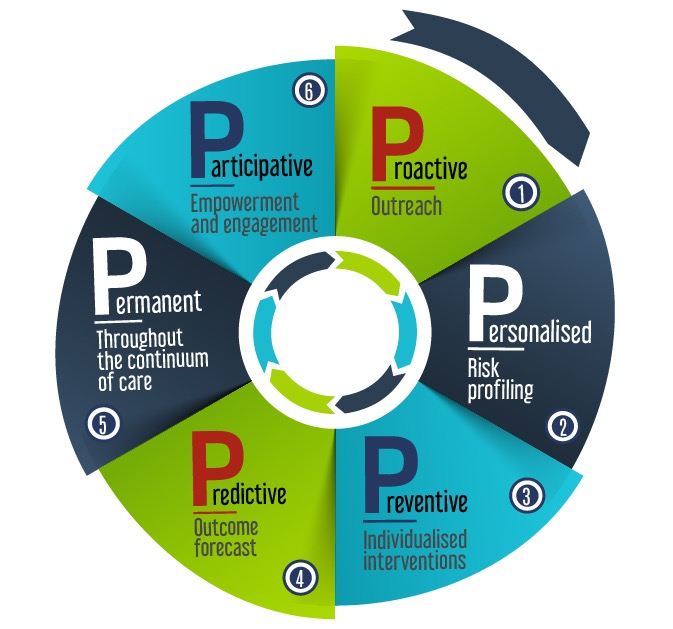
⦁ Personalized, with algorithms that stratify the risk profile based on their health conditions and the environment.
⦁ Preventive, with specific individualized interventions for timely attention to those risk factors, considering their health and their context.
⦁ Predictive, use of AI for the prediction of risks and evolution of the state of health, based on their state of health, their lifestyle and the environment.
⦁ Permanent, ensuring the provision of services through continuous care, in both the different levels of care and in time.
⦁ Participative, with strategies that empower patients and empower them in the care of their health.
Impact of Digital Health on universal health coverage
Digital Health permits universal health coverage, advancing the fulfillment of the U.N. Sustainable Development Goals through the following:
⦁ Reengineering of processes: the accelerated introduction of innovations permits efficient and effective healthcare services.
⦁ Expert systems: use of algorithms that support clinical decision making.
⦁ Supply chain: traceability and tracking of medicines, vaccines, lab tests and health products in the different points of the health system.
⦁ Continuing education: Use of learning platforms that facilitate the quick adoption of the latest advances in prevention, diagnosis and care, reaching remote communities.
⦁ Monitoring of performance: monitoring of the effectiveness and quality of the health services provided, on a population basis.
⦁ Financing for results: selection of the most cost-effective interventions, with incentives for fulfillment.

References
- In the framework of the 71st World Health Assembly in May 2018, the World Health Organization (WHO) published a resolution that emphasizes the role of Digital Health in the transformation of health systems. Since then, the WHO has created the Digital Health Department, has designated a Head of Scientific Data, has created a Digital Health Technical Advisory Group, and has launched the Digital Health Strategy 2020-2025.
- In October 2016, the Pan American Health Organization (PAHO) published the document “eHealth in the Region of the Americas: breaking down the barriers to implementation”. A month later it announced the initiative called “Information Systems for Health (IS$H)”, and in July 2018 it launched the course titled “eHealth for managers and decision makers” intended for decision makers that wish.
- The Broadband Commission for Sustainable Development formed a Digital Health Working Group to encourage a robust agenda on Digital Health with decision makers of the public and private sectors. Since 2017, the Commission has published three iconic reports: Digital Health: A Call for Government Leadership and Cooperation between ICT and Health (2017), The Promise of Digital Health: Addressing Non-Communicable Diseases to Accelerate Universal Health Coverage (2018); and Reimagining Global Health through Artificial Intelligence: the Roadmap to AI Maturity (2020).
- In 2011, the Inter-American Development Bank (IDB), through the Meso-American Health Initiative, and with the support of the Carlos Slim Foundation and the Bill and Melinda Gates Foundation and the Government of Spain, began supporting the participating countries in the development and implementation of Digital Health solutions, especially in the Central American countries. In parallel, the Social Protection and Health Division has been financing and providing technical support to the countries that wish to implement Digital Health Solutions. In 2019, the IDB launched +Digital, a platform that emulates the Health Atlas of the WHO, where the different applications of Digital Health in the region are shown.
- Tapia-Conyer, Roberto and Saucedo-Martínez, Rodrigo. “La Salud Digital: Eje de la Transformación del Sistema de Salud de México”, in Contreras Bustamante, Raúl and Peñaloza, Pedro José (coords.) ¡Sí hay salidas! México: Universidad Nacional Autónoma de México and Editorial Porrúa 2018.
- The term “personalized public health” was coined by Roberto Tapia-Conyer and it is constructed on the principles of population health which, thanks to Digital Health, can be personalized and designed for the specific needs of each person, based on the scientific advances of genomics, metabolomics, proteomics, the current state of health and the health determinants, among others.